Bidirectional Influence between Gut and Brain
The gut-brain axis is a fascinating bidirectional communication network that connects the enteric and central nervous systems. Not only is it anatomical, but it also includes endocrine, humoral, metabolic, and immune routes of communication. This intricate network allows the brain to influence gut activities, including immune response, while the gut can influence mood, cognition, and mental health.
Numerous studies have shown that the enteric microbiota plays a profound role in shaping the gut-brain relationship. Fluctuations in the microbiota have been linked to changes in emotional and cognitive centers of the brain, and they are associated with various mood disorders such as anxiety, depression, and autism spectrum disorders. Conversely, functional gastrointestinal disruptions often have psychological comorbidities related to alterations in the gut microbiome.
Pathways of the Gut-Brain Axis
One significant pathway of the gut-brain axis is the neurologic pathway, which involves the vagus nerve, the enteric nervous system, and neurotransmitters in the GI tract. These pathways produce molecules that can act as local neurotransmitters and influence gut-brain communication. Additionally, gut microbiota can affect brain plasticity and the physiological response to stress.
Another important pathway is the endocrine pathway, where gut microbiota influences the release of biologically active peptides from enteroendocrine cells. This affects the gut-brain axis, impacting critical neurobiological functions such as mood regulation, sleep-wake cycle, and feeding behavior.
The humoral/metabolic pathway is influenced by bacterial metabolites, particularly short-chain fatty acids (SCFAs), which have hormone-like activity and immunomodulatory properties. SCFAs interact with nerve cells and can cross the blood-brain barrier, regulating microglia homoeostasis and affecting behavior modulation. Dysbiosis can disrupt SCFA metabolism, potentially contributing to conditions like autism.
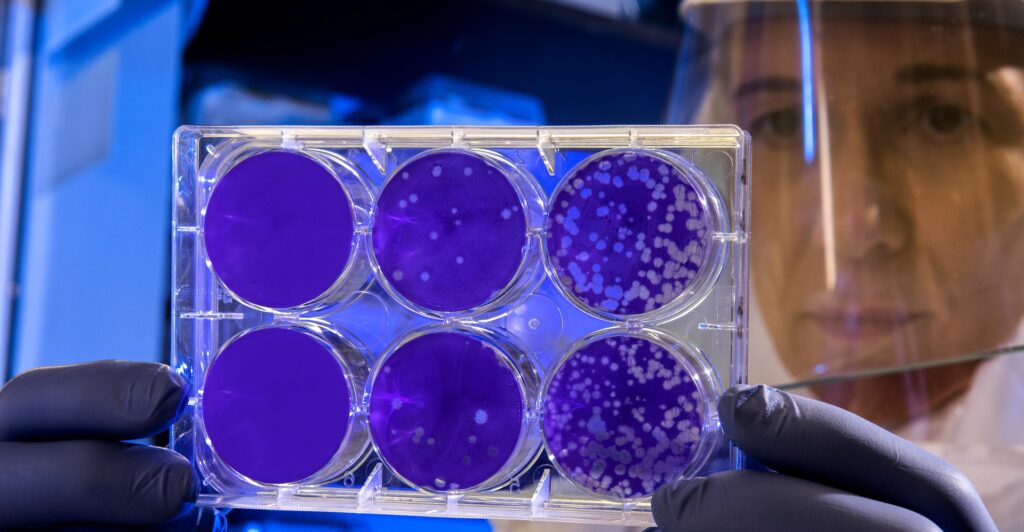
Lastly, the immune pathway plays a role in inflammation metabolism within the GI tract. Gut microbiota can modulate the release of cytokines and cellular communication mediators, affecting gut-brain communication. Inflammatory phenotypes have been linked to depression, and the microbiome and probiotics have shown promise in managing inflammatory conditions.
Probiotics For Treating Mood Disorders
Research on the gut-brain axis has paved the way for investigating the use of probiotics for treating mood disorders in humans. Understanding the complex interactions between gut microbiota and the brain may open up new avenues for preventing and treating conditions like depression by targeting the gut microbiome. As the research on this fascinating topic continues, the potential for improving mental health through gut health becomes increasingly evident.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/